The cornea is the clear, outermost portion of the eye. It is known as the “window” of the eyeball. The cornea is made up of 4 layers. A corneal ulcer is an abrasion or erosion of the cornea. Corneal ulcers are classified by the depth of corneal involvement and by their underlying cause. Causes of corneal ulcers include eyelash abnormalities, eyelid abnormalities, disorders of the tear film (e.g. dry eye disease), infection (bacterial and/or viral), trauma, and chemical irritants.
For the successful management of corneal ulcers, the inciting cause of the ulcer is identified and addressed, the severity of the ulcer is determined, and the appropriate therapeutic modality is selected (e.g. medical management +/- surgical intervention).
Classic superficial corneal ulcer (uncomplicated)
Uncomplicated superficial corneal ulcers typically heal within 5-7 days. A topical antibiotic should be given three to four times daily to prevent secondary bacterial infection during the healing process. Depending on the degree of discomfort, a systemic pain medication should and/or topical dilating medication (e.g. atropine) can also be considered. An Elizabethan collar (E-collar) is necessary to prevent self-trauma or rubbing of the eye, and to allow for proper healing. If the ulcer does not heal within 7 days, then the eye should be re-examined for any undetected, underlying cause of the corneal ulcer.
Indolent corneal ulcer
Uncomplicated superficial corneal ulcers typically heal within 5-7 days. A topical antibiotic should be given three to four times daily to prevent secondary bacterial infection during the healing process. Depending on the degree of discomfort, a systemic pain medication should and/or topical dilating medication (e.g. atropine) can also be considered. An Elizabethan collar (E-collar) is necessary to prevent self-trauma or rubbing of the eye, and to allow for proper healing. If the ulcer does not heal within 7 days, then the eye should be re-examined for any undetected, underlying cause of the corneal ulcer.
Therapeutic interventions are aimed at removing the redundant corneal epithelium and debriding the abnormal cornea. Corneal debridement using cotton-tipped applicators (CTA), or Q-tip, can be a sole therapy, and is often the initial step for treatment of an indolent corneal ulcer. The overall success rate of CTA epithelial debridement alone is approximately 50%. A variety of additional treatments for indolent corneal ulcers include diamond burr debridement and grid keratotomy. Success rate for both of these procedures, in addition to CTA, is about 70-90% within 2-3 weeks. A contact lens may be placed to attempt to facilitate healing and comfort. The efficacy of the role of the bandage contact lens in terms of healing is variable among several studies.
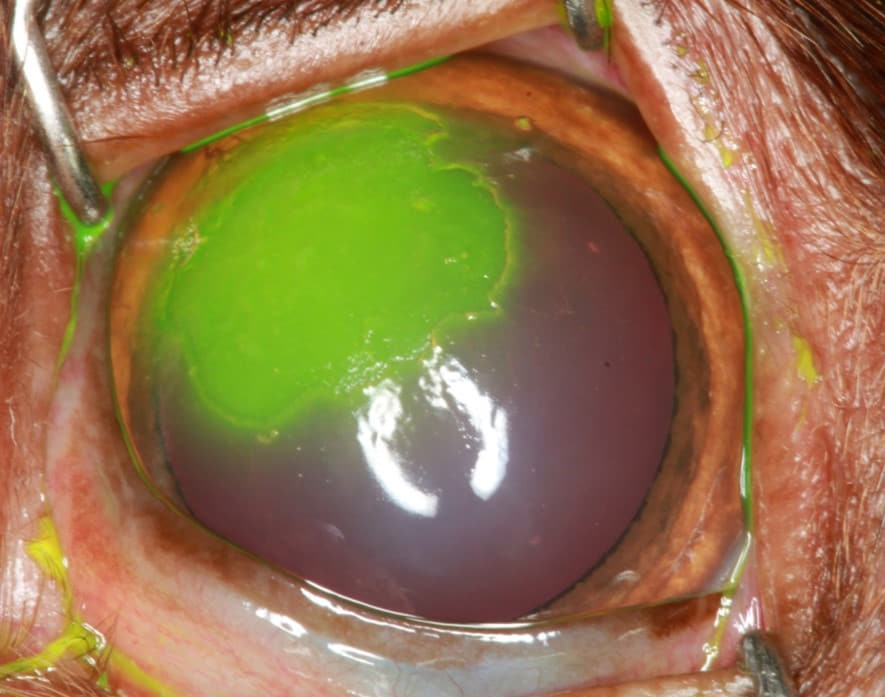
Figure 1. Indolent corneal ulcer exhibiting classic redundant, nonadherent corneal epithelial margins
Medical treatment recommendations for indolent corneal ulcers are the same as for classic superficial corneal ulcers with the exception of a systemic pain medication always being recommended due to the increased degree of discomfort associated with the debridement procedure(s).
Deep corneal ulcer
Any corneal ulcer with suspicion of depth or infection should not be debrided due to risk of seeding infection deeper into the cornea and/or increasing the risk of corneal perforation. In general, ulcers develop depth when they are complicated by bacterial infection. A culture sample should be collected in any eye with signs of infection. Broad spectrum topical antibiotic therapy should be started right away, and can be altered as needed based on the results of the culture and susceptibility testing. A dilating agent and systemic pain management should also be given. The goal of medical treatment is to address infection and inflammation to give the cornea time to heal itself. The main risk of deep ulcers is corneal perforation or rupture.
Surgery is typically recommended for an ulcer greater than 50% corneal depth, and quick referral to an ophthalmologist is important for the best prognosis. The most common surgery for deep ulcers is a conjunctival pedicle graft. The function of the graft is to provide protection and tectonic support while the defect heals. Additionally, blood supply through the graft, which otherwise might not reach the defect for days to weeks, will deliver important factors for healing and can help deliver systemic antibiotics to the site, in addition to topical therapy. These properties of a graft make it favorable that it will help to heal the defect more quickly than medications alone.
Patients with deep ulcers that are quickly referred to an ophthalmologist for surgery typically have a good prognosis for continued vision and comfort in the affected eye pending post-operative healing. Post-operative complications include graft dehiscence due to persistent infection or due to self-trauma, which is why it is imperative that the patient wear the E-collar at all times.

Figure 2: Corneal perforation
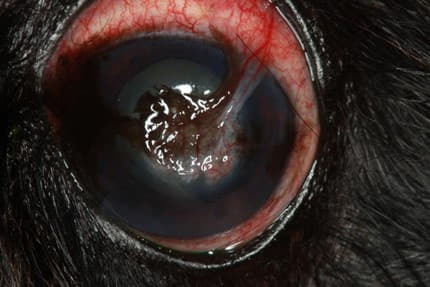
Figure 3. Conjunctival pedicle graft performed for the corneal perforation shown in Figure 2
